Abstract
Background: Outcomes disparities of African American (AA) patients with diffuse large b-cell lymphoma (DLBCL) is heterogeneous and poorly understood. AA patients present at a younger age, often have more aggressive features and inferior clinical outcomes when compared to non-AA patients. Molecular features and clinical prognostic tools conventionally used to risk stratify disease outcomes would not accurately predict survival in black patients. Here, we describe clinical and disease factors associated with worse survival in AA patients with DLBCL.
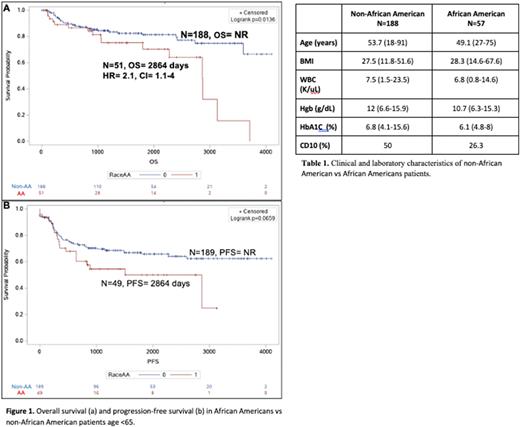
Methods: For this study, we conducted a retrospective analysis of patients who were treated for diffuse large b-cell lymphoma (DLBCL) at Baylor St. Luke's Medical Center (BSLMC) and Ben Taub General Hospital in Houston, Texas. Inclusion criteria were DLBCL diagnosis confirmed by pathology and age between 18 and 65 years (y). Patient's self-reported race was obtained from the patient's medical record. CD10 positivity was detected by immunohistochemistry or flow cytometry of obtained biopsies. SAS statistical software was used for all analysis. Patient demographics, disease characteristics and clinical outcomes were summarized through descriptive statistics. Cox regression model was used to evaluate independent variables effects on overall survival (OS) and event-free survival (EFS).
Results: We identified 288 patients with DLBCL, of which 57 self-identified as AA. At the time of treatment, the median age of Non-AA patients was 53.7 (y) compared to 49.1 y in black patients. A higher percentage of AA patients had a BMI>35 (31.4% vs 18.8%, p=0.05) and lower hemoglobin (mean 10.6 g/dL vs 12.1 g/dL, p=0.002) compared to non-AA patients. Bone marrow involvement at time of diagnosis was seen in 14.4 % in non-AA patients and 24% AA patients (p=0.2). Fewer AA patients had disease with CD10 expression (26.3% vs 50%, p=0.05). The percentage of patients with high-risk international prognostic index (IPI) scores were similar between AA patients and Non-AA patients, 19.8% and 34.7% respectively (p=0.6). Compared to age-matched non-AA patients, AA patients <65 y old had worse OS than non-AA, median survival of 8.0 years and was not reached, respectively. (p=0.01) (Fig 1) Cox regression demonstrated independent additive effect of anemia (p=0.006) on AA inferior outcome.
Conclusion: Our data demonstrates that anemia, is associated with inferior survival in AA patients with DLBCL. Pre-treatment anemia has been previously shown to negatively impact survival in DLBCL and aligns with the outcomes of AA patients in our cohort. Albeit lack of CD10 expression and severe obesity may correlate with adverse outcome, larger data is needed to reconfirm these observations. Our study validates several previously reported risk factors associated with worse survival in AA patients with DLBCL. Studies are needed to better delineate nontraditional/genomic factors underlying the outcome disparities in AA patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.